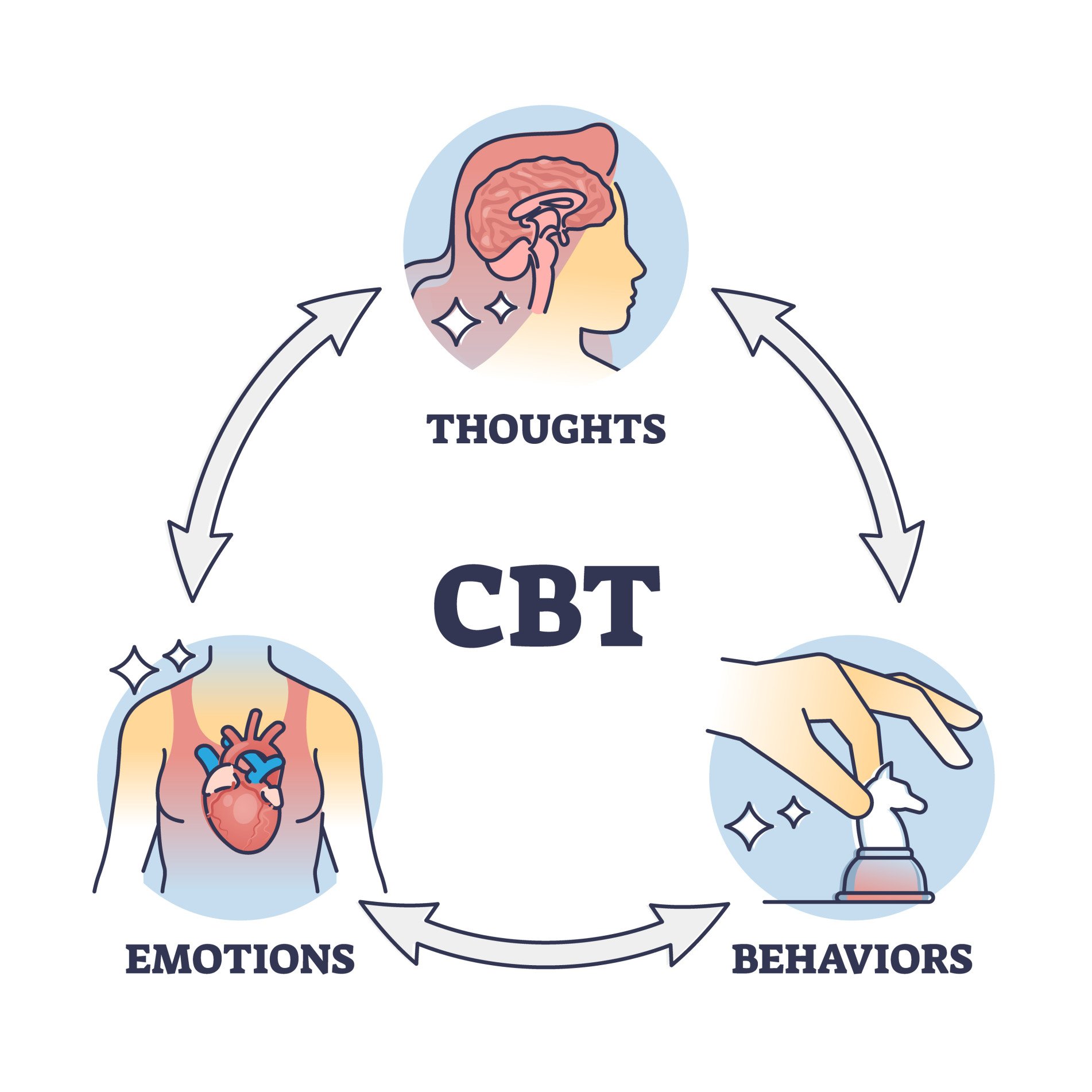
Cognitive Behavioural Therapy (CBT) is a talking therapy that can help clients to manage problems by changing the way they think and behave.
CBT is based on the concept that thoughts, feelings, physical sensations and actions are interconnected, and that negative thoughts and feelings can create a negative cycle.
CBT aims to help clients deal with overwhelming problems in a more positive way by breaking them down into smaller parts. Clients are shown how to change these negative patterns to improve the way they feel.
CBT has been shown to be an effective way of treating a number of different mental health conditions.
What will the Journey look like?
Treatment starts with assessment which allows you and your therapist to get a good understanding of your issues and how these may have developed. You can then explore together how they affect your life, and what keeps them going. Although we may talk about past experiences, CBT is structured to work in the here and now.
You may be offered individual sessions or therapy as part of a group. If you have access to a computer or smart device you may be offered the option to attend virtually.
Will it work for me?
NICE (National Institute of Clinical Excellence) recommends CBT as an excellent therapy with great success in addressing issues such as anxiety and depression. Sometimes a combination of medication and CBT can also lead to good results; your therapist will discuss this with your during your assessment and treatment.
We understand that finding new ways of coping with distressing thoughts can be upsetting at times. Your therapist will guide you through this in a sensitive and caring way with support available. Staff in the Southern Trust CBT Team are fully qualified CBT therapists, and this means you can be assured you are receiving the best evidence-based care and treatment.
What does a CBT session look like?
Typically CBT sessions might involve:
Discussing problems that you want to work on
Setting specific goals to work towards
Exploring thoughts, feelings, and behaviours (sometimes using charts, whiteboards or diagrams)
Practising skills you have learned during and between sessions, or reading material that will help you better understand your situation.
Sessions are weekly and last 50 minutes. We will agree together tasks for completion at home, and this may involve recording things like thoughts, moods or other activities for discussion at the next session.
A really important part of CBT is working together with a therapist to address your difficulties and set goals you think are important.
How many sessions will I need?
After your assessment your therapist will discuss a specific treatment plan for your needs and this can be between 6 and 20 sessions. To benefit from CBT, you will need to be prepared to attend sessions on a regular basis.
Who will deliver my treatment?
The Southern Trust CBT service staff provide treatment and are all fully qualified trained and accredited CBT therapists. This means you can be assured you are receiving the best evidence based delivery of care and treatment
In line with Stepped care model patient presentation requires Step 3 CBT intervention, following NICE guidance as below:
Referrals to Cognitive Behavioural therapy must be able to meet the following criteria:
In addition, individuals are likely to gain most from a cognitive behavioural approach if:
Many of the above listed individual characteristics are likely to support any therapeutic approach. However, they are perhaps particularly relevant in the case of CBT, where heavy emphasis is placed on the patient working actively towards change. These features must be considered with the specific defined problem, to determine suitability.
Presenting Conditions
Specific conditions that may be appropriate for Cognitive Behavioural Therapy include:
For all needle/blood phobias- This type of referral is required to be seen in a medical facility/ Bluestone Unit. Arrangements need to be made to book room and secure a personal alarm for staff in case a Crash trolley is required.
Evidence based models support the use of CBT as an effective treatment choice for psychosis and Bi-polar disorder. However further training updates are required to deliver these. Currently SHSCT CBT staff are unable to treat this client group until training is complete. These criteria will be reviewed accordingly.
Referrals that would not be appropriate for Cognitive Behavioural Therapy include those for individuals where the presenting/primary problem is;
Referrals accepted form GP Via: CCG and internally from other trust services.
Consent must be sought from service user to make referral.
Appointments can be offered virtually via MS Teams, telephone or in person in CBT service premises.
** Clients may be offered an appointment in any facility in Southern Trust area, this helps to reduce the waiting times.**
Monday – Friday 9:00am - 5:00pm
Excluding Bank and Public holidays
028 3824 7537